
OUR PAST PROJECTS
ARMD: ANALYSIS OF GENE EXPRESSION IN THE HUMAN RETINA
Age related macular degeneration: analysis of gene expression in the human retina
A genetic origin of the Age-Related Macular Degeneration (ARMD) has been inferred (genes of the immune system, H-factor of the complement, etc.), but related studies have so far been carried out in the genome of peripheral blood cells and never in ocular tissues. The reasons behind this are the huge practical difficulties encountered in obtaining human retina/choroid samples for research purposes, and in rapidly processing the genetic material extracted from these samples. The aim of this research project was to study potential alterations in gene expression directly in the retinal/choroid tissues of subjects affected by ARMD.
SPONSOR: Global Ophthalmology Awards Program from BAYER
PARTNERS INVOLVED: University of Parma (Italy)
bEYElateral STEM CELL
Regeneration of ocular surface in patients affected by bilateral stem cell deficiency in corneal limbus: comparative efficacy analysis of between buccal mucosa’s stem cell and conjuntiva epithelial stem cell
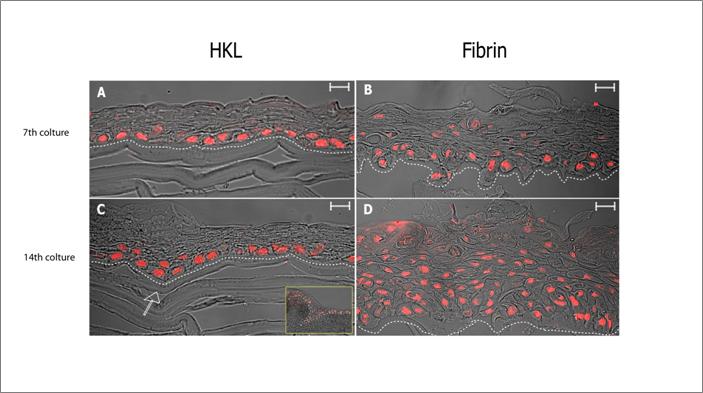
The stem cells of the corneal epithelium are located in the limbus. Pathologies/injuries affecting the limbus lead to limbal stem cell deficiency (LSCD) and eventually vision loss. In the last 10 years, reconstruction of the ocular surface using transplantation of corneal epithelial stem cells (SCs) isolated from limbal biopsies and expanded in vitro has proven to be successful, with 70% of patients showing disappearance of clinical symptoms and restoration of visual acuity. However, in patients with bilateral LSCD (no limbus left on both eyes) transplantation of donor-derived cultured limbal SCs is limited by the side effects of immunosuppressants. The goal of this proposal was to develop new therapies based on transplantation of autologous SCs from alternative sources (oral mucosa and conjunctiva) and to evaluate whether they can reprogram/differentiate into corneal epithelial SCs and generate tissue-engineered cell sheets able to reconstruct the corneal epithelium.
SPONSOR: Veneto Region
PARTNERS INVOLVED: “Alto Vicentino” ULSS4 Hospital, ULSS12 Hospital and Azienda Ospedaliera Universitaria Integrata di Verona

TARGETING CONNEXIN 43 BY GENE THERAPY FOR SCAR REDUCTION AND REGENERATIVE HEALING OF HUMAN CORNEA
Marie Curie COFUND Programme
The cornea serves as a barrier and contributes to the maintenance of corneal transparency necessary for good vision. In most cases, injuries resulting in corneal defects are recovered promptly. Conventional treatment with Mitomycin C or 5-Fluorouracil can reduce the inflammation but the side effects are potentially sight threatening. Procedures such as anterior lamellar keratolplasty, commonly performed by the Veneto eye bank, selectively replace the injured front part of the cornea. This project aims at using gene therapy to target connexin 43 (Cx43) gene expression for reducing inflammation and accelerating wound healing after transplantation of corneas to improve corneal graft survival rates. Additionally, scar formation exerts negative effects on the vision and severe scars may require allograft transplantation. Reduction of scar formation via improved wound healing is an ideal solution for these patients.
SPONSOR: FP7 Marie Curie COFUND Programme
PARTNERS INVOLVED: University of Perugia
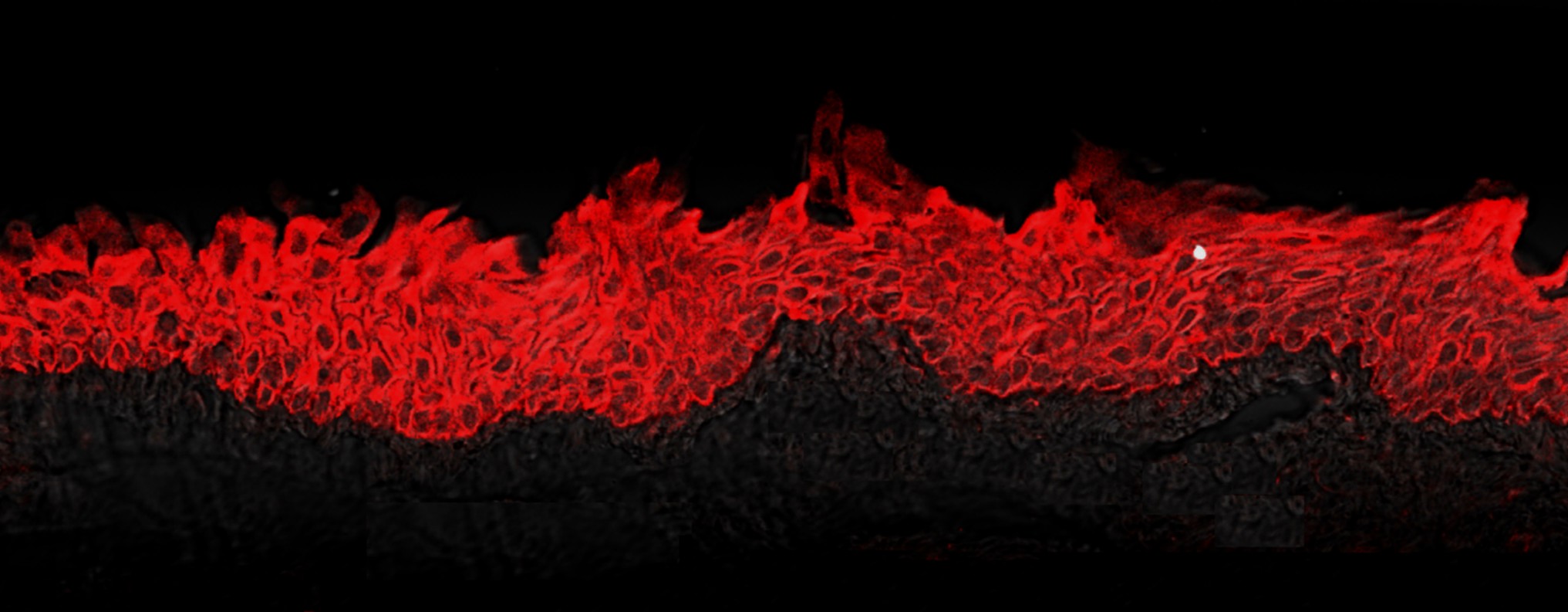
LSCD: TOWARDS A TISSUE ENGINEERED HEMICORNEA
Innovative method for the treatment of total limbal stem cells deficiency (LSCD) through a tissue engineered hemicornea
The principal goal of this project was to evaluate an innovative and single-stage approach for the treatment of visual impairment due to corneal opacities in patients with LSCD. The aim was (i) to reconstruct an innovative human corneal tissue-engineered (hemicornea) in vitro, containing autologous limbal stem cells, directly cultivated onto a corneal stroma obtained by human donor keratoplasty lenticules (HKLs) and (ii) to test the efficacy of this new approach of tissue engineering in patients suffering from LSCD through a single-stage surgical procedure termed keratolimbal autograft combined with anterior lamellar keratoplasty.
To achieve this goal the Veneto Eye Bank Foundation (FBOV) collaborated with the IRCCS G.B. Bietti Foundation of Rome, and with two eye surgeons (Dr. Galan of S. Antonio Hospital, and Prof. Busin of Villa Serena Hospital) with long term experience in PK and limbal stem cell transplantation.
SPONSOR: Ministry of Health
PARTNERS INVOLVED: University of Padova, IRCCS Fondazione G. Bietti Onlus, ULSS16, Villa Igea Hospital
MESENCHYMAL STEM CELLS FOR CORNEA REGENERATION
Use of human bone marrow mesenchymal stem cells for bone and cornea regeneration and for the treatment of GVHD after haemopoietic stem cell allotransplantation (Italy)
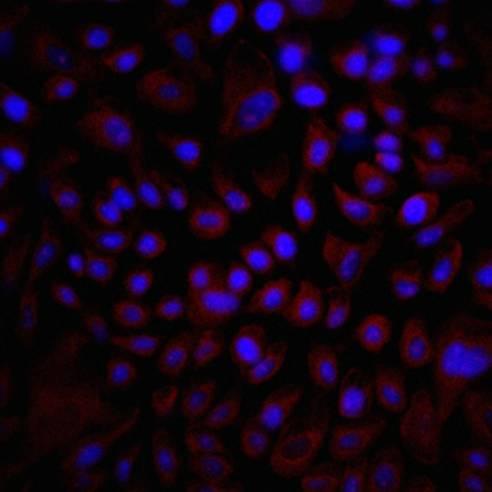
Corneal epithelial stem cells are localized in the limbus, an anatomical structure that circumscribes the cornea and separates it from the conjunctiva. Limbal stem cell deficiency (LSCD) caused by endogenous diseases or corneal epithelium injuries results in complete destruction of corneal epithelium generating conjunctivalization, chronic inflamation, neovascularization, opacification and continuous ulceration of the cornea, which in turn leads to a chronic pain, photophobia, dry eye and, ultimately, to a visual impairment or blindness. Patients with unilateral affection of LSCD can be treated with autologous transplant of LSC taken from the healthy eye, but this therapeutic approach is not feasible in the case of bilateral affected patients for whom allogeneic LSC transplantation from cadaveric tissue or a HLA-matched donor is the current therapeutic strategy. Allogeneic transplantation is far from being an optimal treatment since it requires prolonged systemic immunosuppression, leading to side-effects such as disorders of liver and renal function, arterial hypertension, bone marrow depletion and neurotoxicity, which compromise the life quality of patients. Moreover, despite of immunosuppression, the success rate of grafting tends to decrease gradually over time (graft survival rate of 40% at 1 year, and 33% at 2 years).
Bone marrow-derived mesenchymal stem cells (BMMSC) are pluripotent cells distinct of the hematopoietic lineage cells with the capacity to differentiate to osteoblasts, chondrocytes and adipocytes. Also, BMMSC have been shown to transdifferentiate into extramesenchymal lineages like endoderm and ectoderm, a level of plasticity characteristic of embrionic stem cells (ESC). However, unlike ESC, these adult stem cells have not tumorigenic properties and can be extracted from patients by simple bone marrow aspiration and easily expanded in vitro. These characteristics make BMMSC a perfect target for regenerative therapies based on using autologous stem cells in order to avoid problems derived from the allotransplantation-induced immunorejection and the systemic immunosupression treatments.
SPONSOR: CariVerona Foundation and Veneto Region
PARTNERS INVOLVED: University Hospital of Verona (Italy, LEADER), Vicenza Hospital (Italy)

